Pathogenesis and Symptoms
VOD/SOS is a complex cascade of events that can ultimately lead to death1-4
An in-depth look at the complex pathogenesis of VOD/SOS
VOD/SOS is a post-HSCT complication primarily associated with conditioning regimens that affects the endothelial cells within the sinusoids of the liver1,5
Video Transcript
VOD, also known as sinusoidal obstruction syndrome, is a potentially life-threatening complication of hematopoietic stem-cell transplantation and, in severe cases, is associated with a mortality rate of over 80%.
The pathophysiology of VOD is complex, involving both endothelial cell damage and development of a prothrombotic and hypofibrinolytic state.
It is thought that the initial trigger for the development of VOD is the damage to hepatocytes and activation of sinusoidal endothelial cells in the liver. This is caused by toxic metabolites generated during the conditioning regimen used prior to transplantation.
This endothelial cell injury leads to the expression of adhesion molecules and the release of cytokines and chemokines, which trigger inflammatory pathways that further damage the endothelium.
Activated endothelial cells also release heparanase, which breaks down the extracellular matrix resulting in the loss of cytoskeletal architecture.
Activated endothelial cells begin to round up and gaps form in the endothelial lining.
Red blood cells, leukocytes, and cellular debris pass through these gaps and accumulate in the space of Disse, leading to narrowing of the sinusoid.
The endothelial cells dissect off and embolize downstream, resulting in blockage of the sinusoid and ultimately to reduced hepatic venous outflow.
VOD is also characterized by a prothrombotic and hypofibrinolytic state, in which an increase in tissue factor and plasminogen activator inhibitor 1 contributes to increased fibrin deposition and clot formation. This eventually leads to obstruction of the sinusoids.
VOD/SOS can progress from endothelial cell damage to multi-organ dysfunction and death1-4
Based on experimental models, buildup of toxic metabolites from conditioning regimens may trigger damage to sinusoidal endothelium1-4
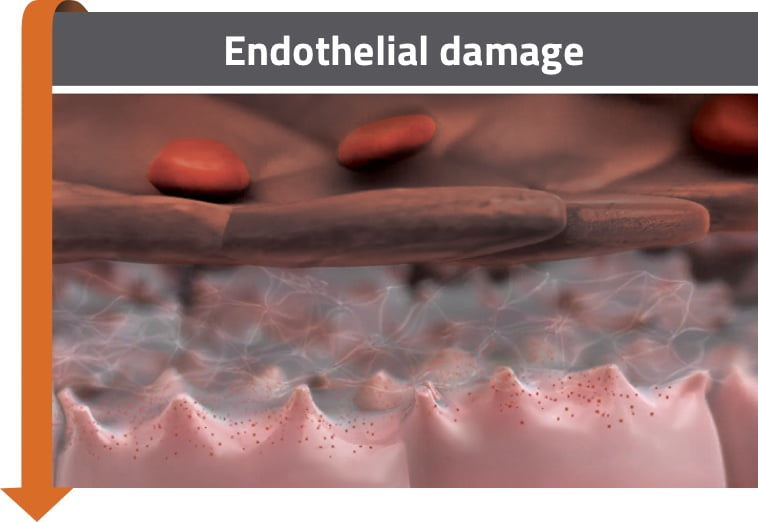
- Activation of pro-inflammatory mediators may lead to sinusoidal endothelial cell damage3,4
- Heparanase contributes to degradation of the extracellular matrix and gap formation between sinusoidal endothelial cells2,4
- Degradation of the extracellular matrix leads to detachment of endothelial cells from the sinusoidal lining6,7
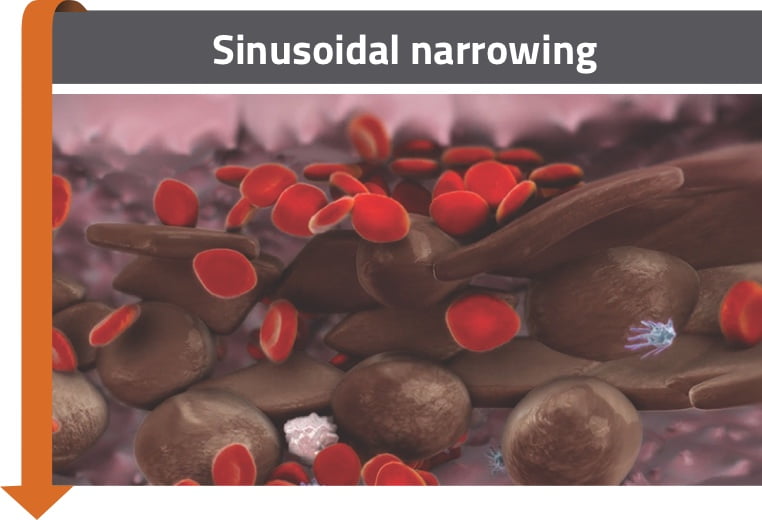
- Red blood cells, leukocytes, and cellular debris accumulate in the space of Disse2-4
- This can lead to sinusoidal narrowing and dissection of endothelial cells, which may embolize downstream and contribute to sinusoidal blockage2-4
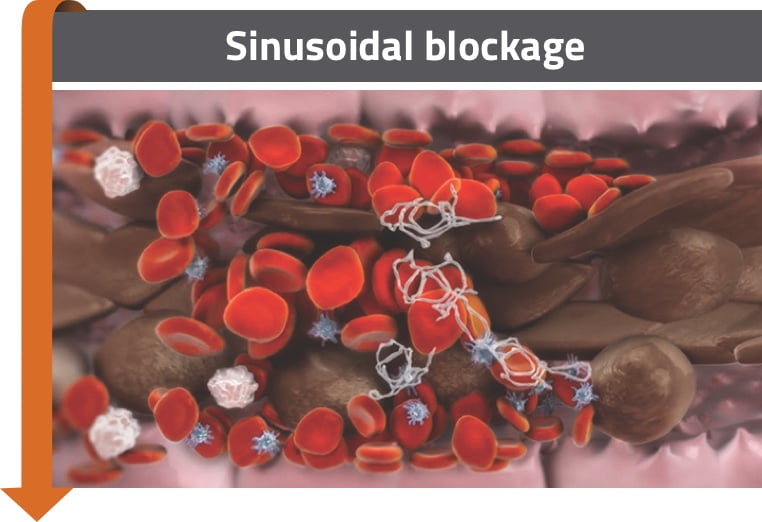
- Expression of factors that regulate coagulation and fibrinolysis contributes to a procoagulant and hypofibrinolytic state1,3,4
- Fibrin deposition, clot formation, and embolization of dissected endothelial cells can cause blockage1,3,4
- Hepatocyte cell death is a consequence of sinusoidal disruption2,3,5
- May lead to a reduction in hepatic venous outflow and to post-sinusoidal hypertension2-4
The cascade of events appears to start before clear clinical and laboratory manifestations are evident3,4,8
Severe liver dysfunction can be the result of the cascade of events in VOD/SOS1-4,6,8-10
Endothelial damage
Sinusoidal narrowing
Sinusoidal blockage
Reduction of hepatic venous outflow
Post-sinusoidal portal hypertension
Multi-organ dysfunction
Not all patients progress to multi-organ dysfunction and death
Death
Most common signs and symptoms2,8,11
- Weight gain due to fluid retention
- Hepatomegaly
- Right upper quadrant pain
- Elevated bilirubin
- Elevated serum transaminase and alkaline phosphatase
- Ascites
- Excessive platelet transfusions consistent with refractory thrombocytopenia