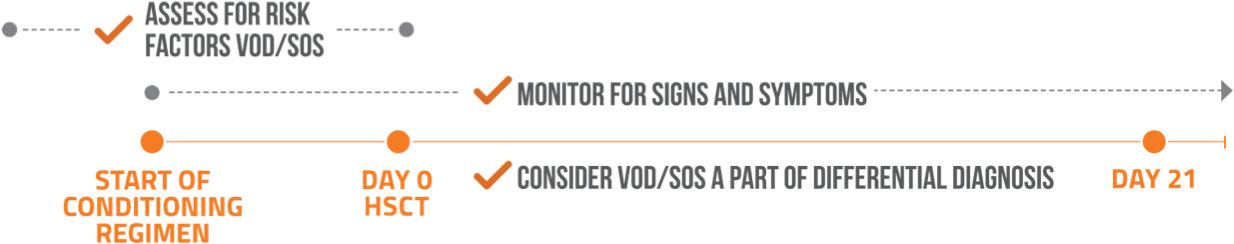
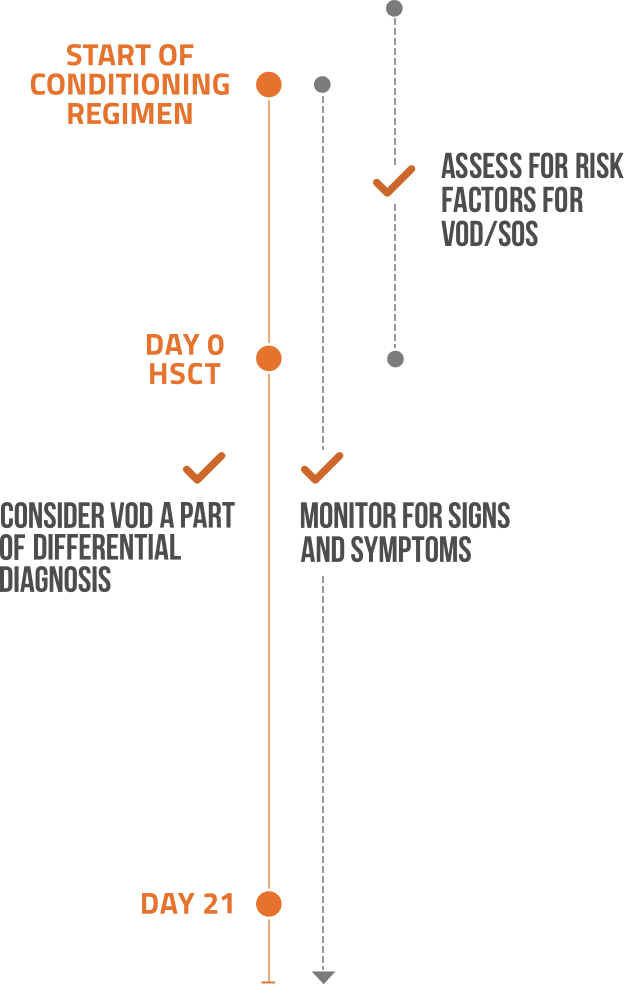
HSCT=hematopoietic stem-cell transplantation; SOS=sinusoidal obstruction syndrome; VOD=veno-occlusive disease.
References: 1. Carreras E. How I manage sinusoidal obstruction syndrome after haematopoietic cell transplantation. Br J Haematol. 2015;168(4):481-491. 2. Dalle JH, Giralt SA. Hepatic veno-occlusive disease after hematopoietic stem cell transplantation: risk factors and stratification, prophylaxis, and treatment. Biol Blood Marrow Transplant. 2016;22(3):400-409. 3. Carreras E. Early complications after HSCT. In: Apperley J, Carreras E, Gluckman E, et al, eds. The EBMT Handbook. 6th ed. Paris, France: European School of Haematology; 2012:176-195. 4. Mohty M, Malard F, Abecassis M, et al. Revised diagnosis and severity criteria for sinusoidal obstruction syndrome/veno-occlusive disease in adult patients: a new classification from the European Society for Blood and Marrow Transplantation. Bone Marrow Transplant. 2016;51(7):906-912. 5. Corbacioglu S, Carreras E, Ansari M, et al. Diagnosis and severity criteria for sinusoidal obstruction syndrome/veno-occlusive disease in pediatric patients: a new classification from the European Society for Blood and Marrow Transplantation. Bone Marrow Transplant. 2018;53(2):138-145. 6. Cairo MS, Cooke KR, Lazarus HM, et al. Modified diagnostic criteria, grading classification and newly elucidated pathophysiology of hepatic SOS/VOD after haematopoietic cell transplantation. Br J Haematol. 2020;190(6):822-836. 7. Mahadeo KM, Bajwa R, Abdel-Azim H, et al; Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network; Pediatric Diseases Working Party of the European Society for Blood and Marrow Transplantation. Diagnosis, grading, and treatment recommendations for children, adolescents, and young adults with sinusoidal obstructive syndrome: an international expert position statement. Lancet Haematol. 2020;7(1):e61-e72. 8. Dalle JH, Giralt SA. Hepatic veno-occlusive disease after hematopoietic stem cell transplantation: risk factors and stratification, prophylaxis, and treatment. Biol Blood Marrow Transplant. 2016;22(3):400-409.